Introduction to Corrective Movement Therapies
The notion that you can improve your body and relieve your pain with movement is not a new concept. In fact, Corrective Movement Therapy has been around for thousands of years, just under different names like Yoga and Tai Chi. These practices have been used for centuries to improve the health and wellness of the participants. Because these ancient mind-body practices developed long before the advent of the scientific method, they are enmeshed in a more in a spiritual holistic premise, as were many of the medical practices of the time.

In the development of the reductionistic scientific methods of modern medicine these types of therapies were virtually ignored by the mainstream until fairly recent. The challenge with these methods wasn't that they didn't work, it's just that they couldn't be explained in terms of a paradigm that only examined conditions based on parts.
For instance, from a reductionistic viewpoint scoliosis is viewed as simply a disfigurement of the spine. In reality, the condition called scoliosis encompasses much more than just the spine so treatment requires a whole body approach, rather than just a limited focus on the end result of a twisted spine.
Fortunately, science has begun to catch up to ancient wisdom and can now start to explain in an objective manner how such movements can be beneficial to the body.
Modern Science of Corrective Movement Therapy
Rather than just throwing the baby out with the bathwater a small groups of doctors, scientist and researchers in Eastern Europe in the past century began the scientific study of how movement can be therapeutic for the physical body. Trailblazers in this budding field were rehabilitation greats such as Dr. Karel Lewit and Dr. Vladimir Janda of Prague, Katherina Schroth in Germany in the 1960's through the 1980's. Then later in the West by therapists such as Robin Mckenzie, Gray Cook, and Dr. Craig Liebenson.
While in the United States the scientific approach to Corrective Movement Therapy, also known as Function Movement Therapies are commonly used in rehabilitation of the spine for athletic injuries and repetitive traumas. Yet when it comes to the non-surgical treatment of scoliosis in the U.S., they're almost completely overlooked by Conventional Medicine.
This is not the case in other countries where scoliosis is managed by multi-disciplinary teams of doctors that are composed of not only orthopedic surgeons but also rehabilitation specialists. The general rule of thumb in their step-by-step treatment approach is to start with rehab on one end of the spectrum and if all else fails then scoliosis surgery is recommended on the other end.
Current Conventional Medical Treatment of Scoliosis In the U.S.
In the US, medical management of scoliosis is very "orthopedic-centric", although that's beginning to change. The orthopedic surgeon's paradigm of care focuses on surgery to shore up the structural deficits in the spine with surgical implants of metal rods or external hardware such as a rigid plastic shell brace. Their practice does not usually focus on the rehabilitation of the functional movement patterns that can either drive a curve to progress if ignored or improve if properly stimulated.
 Traditional scoliosis treatment has focused primarily on a forced support of bony scaffolding of the body called the spine and in this approach an external device is applied to the body (either with a hard brace or metal hardware surrounding the spine in a scoliosis surgery) to provide better support. The challenges with this approach are that this type of immobilization causes muscle atrophy and weakness of the muscles supporting the spine and body de-mineralization of the de-weighted bones because the body becomes reliant on the hardware. Also fusing the spine does not stop the forces that were driving the curves to begin with and they continue to cause a slow distortion in the body, especially causing strain at the segments above and below the fused levels.
Traditional scoliosis treatment has focused primarily on a forced support of bony scaffolding of the body called the spine and in this approach an external device is applied to the body (either with a hard brace or metal hardware surrounding the spine in a scoliosis surgery) to provide better support. The challenges with this approach are that this type of immobilization causes muscle atrophy and weakness of the muscles supporting the spine and body de-mineralization of the de-weighted bones because the body becomes reliant on the hardware. Also fusing the spine does not stop the forces that were driving the curves to begin with and they continue to cause a slow distortion in the body, especially causing strain at the segments above and below the fused levels.
Corrective Movement Therapies Specific for Scoliosis
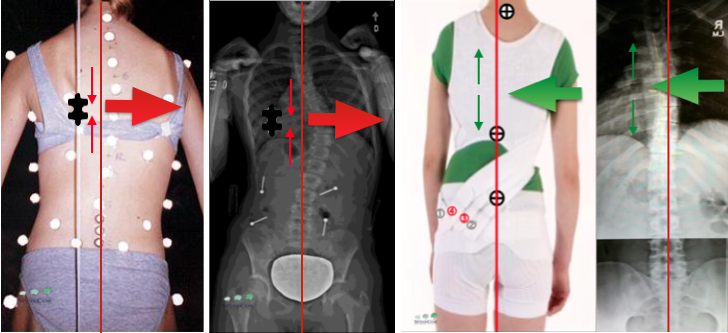
 Scoliosis Specific Exercise applied specifically for you, based on your curve pattern.[/caption]In contrast, Corrective Movement Therapies for Scoliosis actually help provide improved postural support by stimulating the nervous system to activate specifically weakened muscles that are common deficits found in scoliosis. The foundation of these methods were initially developed by one of the pioneer's of the field of Exercise Therapy for Scoliosis, a German Therapist named Katherina Schroth.
Scoliosis Specific Exercise applied specifically for you, based on your curve pattern.[/caption]In contrast, Corrective Movement Therapies for Scoliosis actually help provide improved postural support by stimulating the nervous system to activate specifically weakened muscles that are common deficits found in scoliosis. The foundation of these methods were initially developed by one of the pioneer's of the field of Exercise Therapy for Scoliosis, a German Therapist named Katherina Schroth.
We've incorporated these techniques and enhanced them with more modern concepts of advanced functional movement therapies from around the world and blended them into our unique non-surgical scoliosis treatment approach called Nu-Schroth.
To understand the basis for corrective movement therapies it’s best to first examine how the body changes and mal-adapts in scoliosis to better understand how such specialized treatment works to stop the progression of the curves and even help correct some curves.
Scoliosis Is Controlled By Your Brain
 The nervous system, which is composed of the brain and spinal nerves, is the master control system of the entire body. It not only controls the musculoskeletal system but also the hormonal systems, the cardiovascular, etc. In fact, a branch of science called Neuroskeletal biology that explores the direct influence that the brain has over the growth of the bones in the spine.
The nervous system, which is composed of the brain and spinal nerves, is the master control system of the entire body. It not only controls the musculoskeletal system but also the hormonal systems, the cardiovascular, etc. In fact, a branch of science called Neuroskeletal biology that explores the direct influence that the brain has over the growth of the bones in the spine.
Human evolution has allowed us to develop a finely tuned nervous system that supports our upright posture. Since most of our body mass is an inverted pyramid that sits high above the ground, the balancing act to keep the body balanced is nothing short of amazing.
The spine is the central axis for most movements in the body. It serves both as a stabilization point to allow movement elsewhere in the body. It also is able to move and while the other parts of the body then act as stabilizers of the body. This dual function of the spine to allow both stability and movement is critical to address in the treatment of scoliosis.
When the structural support of this system is undermined the body reacts by developing abnormal patterns of movement and stability that are helpful to keep the body from falling over in the short term but can lead to further worsening of the structural integrity of the spine. This is what can cause progression of scoliosis.
Habitual Patterns of Movement
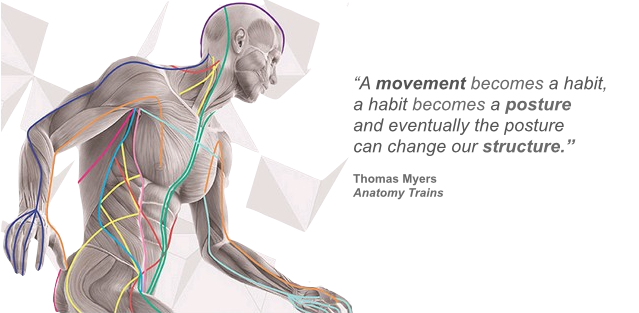
Studies done at the Schroth Institute for Scoliosis in Germany have shown that scoliosis patients all have abnormal movement patterns that can cause their scoliosis to worsen. If these aberrant movement patterns in the brain stay in place long enough they begin to adversely affect the person’s posture.
Postural changes that stay uncorrected will eventually cause structural changes in the body. This is the downward spiral that is commonly found in scoliosis that must be corrected to avoid a future of pain and disability.
In order to reverse this process to improve the structural support of the spine, you must first make postural improvements by re-balancing the muscular movements and stabilization with Corrective Movement Therapy.
Structural vs Functional Scoliosis
Structural scoliosis refers to changes in the shape of the bones of the spine that contribute to a curvature. One extreme example of this would be scoliosis caused by a wedged shaped vertebra. A functional scoliosis is the body's adaptation to an imbalance in the spine or elsewhere in the body.
In reality, most scoliosis has both a structural and functional component of the curves.
The word Correction in Corrective Movement Therapy refers to the restoration of functional support of the spine, which can have quite a profound impact on a functional component of the curve. It can even help improve the structural component of the curve in children who are still growing by helping the delayed side catch up.
Every scoliosis has both a structural and functional component of the curve. The structural component is the body changes that have taken place in the vertebra as a result of the curve causing compression on one side compared to the other. The functional component of the curve is due to the postural collapse over time that due to the failure of supporting tissues.
While a correction in the structure of the vertebra is obviously not available to an adult who has stopped growing, there is still potential for improvement in their scoliosis that can help them relieve their pain and avoid surgery. This is done by helping the brain activate the specifically weakened muscles in the spine and related supporting tissues to help reduce the imbalances in the body that are causing the pain and allowing progression. While the spine of an adult may never be fully corrected, it doesn't have to in order to relieve the pain.
In Adolescent Idiopathic Scoliosis
Research on idiopathic scoliosis has found that during puberty there is often a genetic predisposition for a delay in the growth of the growth plate on one side of a vertebra compared to the other. This precipitates and uneven growth that's what results in the initial tipping of the spine to the side.
This imbalance is further aggravated by the rapid growth taking place around the time of the onset of puberty, which is what causes a rapid progression of scoliosis.
In children who are still growing, the delayed side growth plate of the vertebra can actually be stimulated to catch up with the other side, thus improving the structural deficit with corrective movement therapy.
In Adult Scoliosis
In an adult scoliosis, the structural component of the curve is fairly stationary but the postural component of the curve is changeable. The cause of the postural component of scoliosis in the collapse of the spine due to the uneven forces placed on it by gravity. While scoliosis may look like a simple side-to-side curve on an X-ray, the reality is that it spirals around much like a spring. So if you could imagine a bowling ball sitting on top of a metal spring, you can begin to get a sense of how your scoliosis can gradually collapse over time due to the unrelenting force of gravity.
Once a scoliosis curvature passes 30 degrees gravity really starts to take advantage of it. If the supporting musculature is not strengthened, then the spine will gradually collapse over the years at a slow rate of about 1 degree per year even into adulthood. This can add up to some significant progression of scoliosis over a lifetime. That's why it's still important for adults with scoliosis to regain stability in their spine in the specific weakened areas with properly applied corrective movement therapy.
While movement in the body is caused by muscle contraction it is controlled centrally by the nervous system. The brain controls the posture and movements of the body, so it is the training of the brain that is the focus of our treatment. Both the sensory and motor components of the nervous system are adversely affected in scoliosis.
As scoliosis progresses, especially when it occurs rapidly during adolescence, the brain's sensory-motor network must adapt to these changes. It does this by creating a different map of the body in the brain that doesn't match the reality in the body. This map is known as the Body Schema.
How Your Brain's Map Of The Body Affects Your Scoliosis
Body schema refers to a representation of the positions of body parts in space, which is updated during body movement. When the schema does not match the reality, then the brain's incorrect image of the body's position can reinforce the scoliosis pattern. We see an expression of this quite often when parents bring their child with scoliosis in for an evaluation. They often comment about their daughter's chronically poor posture by saying something like "I always tell her to sit up straight", to which their daughter replies:
"But I AM sitting up straight!"
That's because in her brain the map tells her that her spine is straight so she is sitting up straight when in reality she is not. That habitual disassociation between what's real and what's imagined can lead to progression of scoliosis and must be addressed in treatment.
Also, the autonomic function has found to be dysfunctional in scoliosis with an increase in the sympathetic tone affecting the imbalances in bone growth and should be addressed, especially in growing children.
Balancing the Brain and The Spine With Corrective Movement Therapies
Getting the nervous system back under control is key to helping reduce the scoliosis dysfunctions in the spinal support structures caused by the scoliosis. SpineCor and Schroth designed to help improve the patient’s sensory-motor awareness to allow the body to move back towards mid-line and to activate the deactivated postural muscle in the spine to provide improved postural support and to reduce scoliosis curvatures.
Nu-Schroth Method of Scoliosis Specific Exercise
Scoliosis Specific exercise differs from most other forms of exercise in that it is designed to be corrective only into the direction of correction, where as most other forms of corrective exercises are done bilaterally. The reason that scoliosis corrective exercises need to be done unilaterally instead of bilaterally is that scoliosis already has a profound right to left imbalance in the spine. So while doing one corrective exercise on one side of the body that moves your spine into the direction of correction; doing that exact same exercise going the other way can make your curves worse! So you always only want to do scoliosis exercises into the direction of correction, based on your particular curve pattern.
The Schroth Method is a Corrective Movement Therapy that works by stimulating your brain in a way that allows your body's posture to repeatedly move into the direction of correction using specific postures, breathing techniques and dynamic movements.
This type of corrective movement performed repeatedly overtime is designed to help your body develop new patterns of movement that are corrective. This process allows your brain to begin "recalibrating" to the new corrected position so that it develops a new and improved awareness where the spine should be positioned to help reduce the curves.
The goal is to eventually help you replace your current abnormal movement patterns which are driving your scoliosis curves with new and improved ones that counteract them.
How Can a Scoliosis Brace Be Considered A Corrective Movement Therapy?
When you think of a scoliosis brace you're probably conjuring up an image of a hard plastic shell that immobilizes the spine much like a body cast. When the body is immobilized the muscles are kept from moving, which eventually causes them to atrophy. This is the exact opposite effect that of what happens in corrective movement therapy.
"So how can the SpineCor scoliosis brace be a corrective movement therapy?"
SpineCor is very different than these hard scoliosis braces. Rather than being made of a hard plastic shell, instead, it's made of flexible, elastic bands that wrap around the body in different configurations based on your curve pattern. While you are in SpineCor your body can move whichever direction it likes but it gives your body a gentle reminder to repeatedly move into the direction of correction while you go about your daily activities.
The SpineCor is really more like a rehabilitation device that you wear, in fact, the technical term used to describe SpineCor is an Elastic-Tension Orthosis. That's because the specialized corrective elastic bands that wrap around the body in different configurations based on your curve pattern stimulate particular muscle activation, much in the same way that Kinesio-tape does when applied to the body.
SpineCor's Has Similar Corrective Action to Kinesiotape
What is Kinesiotape?
If you've ever watched the Olympics or professional sports you've probably seen it, you just may not have known what it was.

Kinesio-tape has been used by professional athletes for decades to improve postural correction to allow injuries to heal by stimulating improved “muscle memory” of the supporting muscles to work better. It was because far more widely known since it was first widely recognized during the Beijing Olympics when it helped the US Woman’s Beach Volleyball team of Kerri Walsh and Misty May. Kerri had injured her right shoulder in training so it was taped up before each match to help stimulate the supporting structures in the shoulder to prevent injury. It worked as they won the gold!
By the next time the Olympics came around in London Kinesiotaping was so wide spread among the elite Olympic athletes that you would be hard pressed to find an event where at least one athlete didn’t use it. Clearly it worked, but how?
One explanation involves stimulation of postural muscles in a kinetic chain to work more effectively so that the main mover muscles in an action don’t have to overwork and get injured. It provides the stabilization muscles a gentle reminder to fire when they are needed. It does this by stimulating proprioceptors in the muscles that send information back to the nervous system that they are now in the proper position so that the other muscles in the kinetic chain can react appropriately and not overwork or get injured.
SpineCor - Principle The Same, But The Application Lasts Longer
SpineCor works in much the same way for scoliosis, it’s just far more long lasting then Kinesiotape which has to be changed every 2 -3 days. The elastic bands in SpineCor gives selective muscles in body the same type of gentle reminder to activate to move the body back towards the direction of correction repeatedly throughout the day as it’s being worn while doing your daily activities. Overtime this key repetitive movement results in development of new muscle memory that is corrective for your scoliosis by providing better postural support those weakened muscles that had allowed the collapse of the spine against gravity.
Because these Corrective Movement therapies help the patient make permanent changes in how their body moves and stabilizes itself this allows the patient's body to make changes to make permanent changes in their posture to give them lasting improvements in their scoliosis.
